Caption
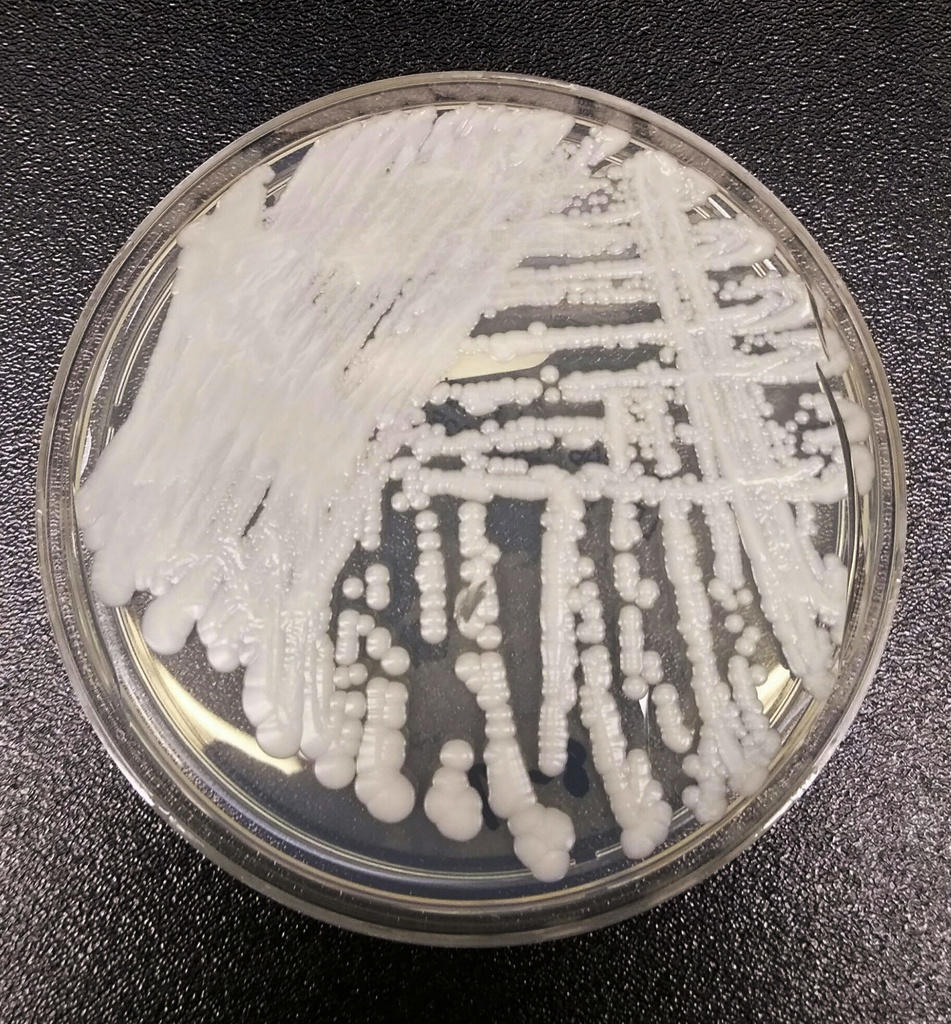
This undated photo made available by the Centers for Disease Control and Prevention shows a strain of Candida auris cultured in a petri dish at a CDC laboratory. In a CDC paper published by the Annals of Internal Medicine on Monday, March 20, 2023, U.S. cases of the dangerous fungus tripled over just three years, and more than half of states have now reported it.
Credit: Shawn Lockhart/Centers for Disease Control and Prevention via AP, File

