Section Branding
Header Content
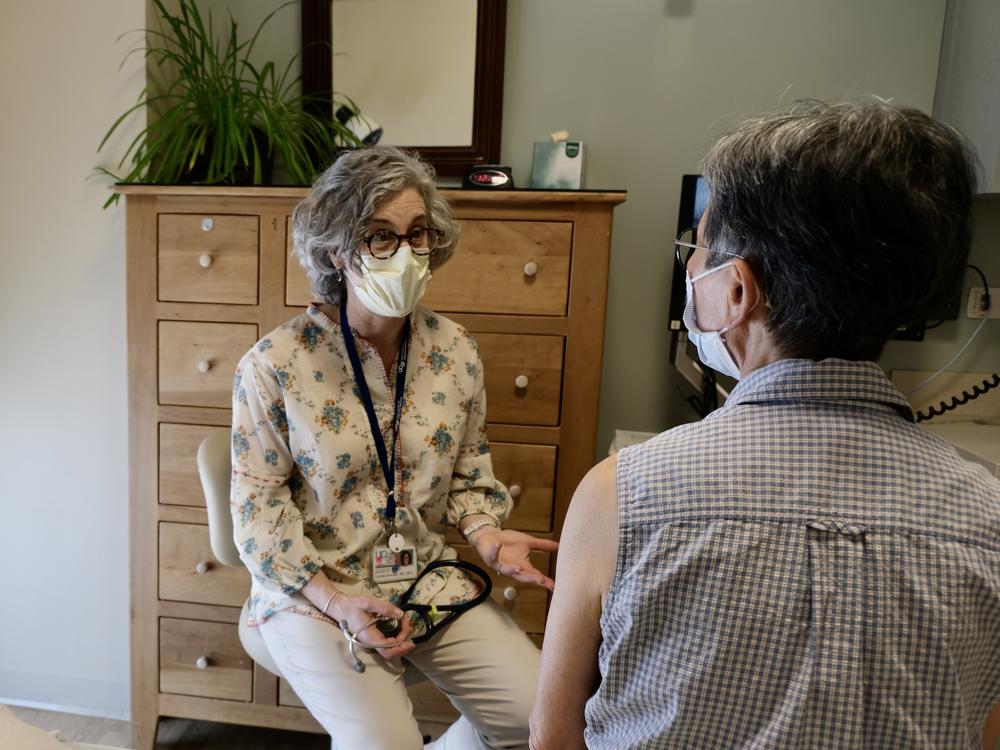
Ageism in health care is more common than you might think, and it can harm people
Primary Content
A recent study found that older people spend an average of 21 days a year on medical appointments. Kathleen Hayes can believe it.
Hayes lives in Chicago and has spent a lot of time lately taking her parents, who are both in their 80s, to doctor's appointments. Her dad has Parkinson's, and her mom has had a difficult recovery from a bad bout of Covid-19. As she's sat in, Hayes has noticed some health care workers talk to her parents at top volume, to the point, she says, "that my father said to one, 'I'm not deaf, you don't have to yell.'"
In addition, while some doctors and nurses address her parents directly, others keep looking at Hayes herself.
"Their gaze is on me so long that it starts to feel like we're talking around my parents," says Hayes, who lives a few hours north of her parents. "I've had to emphasize, 'I don't want to speak for my mother. Please ask my mother that question.'"
Researchers and geriatricians say that instances like these constitute ageism – discrimination based on a person's age – and it is surprisingly common in health care settings. It can lead to both overtreatment and undertreatment of older adults, says Dr. Louise Aronson, a geriatrician and professor of geriatrics at the University of California, San Francisco.
"We all see older people differently. Ageism is a cross-cultural reality," Aronson says.
Ageism creeps in, even when the intent is benign, says Aronson, who wrote the book, Elderhood. "We all start young, and you think of yourself as young, but older people from the very beginning are other."
That tendency to see older adults as "other" doesn't just result in loud greetings, or being called "honey" while having your blood pressure taken, both of which can dent a person's morale.
Aronson says assumptions that older people are one big, frail, homogenous group can cause more serious issues. Such as when a patient doesn't receive the care they need because the doctor is seeing a number, rather than an individual.
"You look at a person's age and say, 'Ah, you're too old for this,' instead of looking at their health, and function, and priorities, which is what a geriatrician does," says Aronson.
She says the problem is most doctors receive little education on older bodies and minds.
"At my medical school we only get two weeks to teach about older people in a four-year curriculum," she says.
Aronson adds that overtreatment comes in when well-meaning physicians pile on medications and procedures. Older patients can suffer unnecessarily.
"There are things...that happen again and again and again because we don't teach [physicians] how to care about older people as fully human, and when they get old enough to appreciate it, they're already retired," says Aronson.
Kris Geerken is co-director of Changing the Narrative, an organization that wants to end ageism. She says research shows that negative beliefs about aging - our own or other people's - are detrimental to our health.
"It actually can accelerate cognitive decline, increase anxiety, it increases depression. It can shorten our lifespans by up to seven-and-a-half years," she says, adding that a 2020 study showed that discrimination against older people, negative age stereotypes, and negative perceptions around one's own age, cost the health care system $63 billion a year.
Still, beliefs can change.
"When we have positive beliefs about age and aging, those things are all flipped," Geerken says, and we tend to age better.
Geerken conducts anti-ageism trainings, often over Zoom, including trainings for health care workers. She also advises older adults on how to push back if they feel their medical concerns are being dismissed with comments like, "It's to be expected at your age."
Age-Friendly Health Systems are another initiative designed to curb ageism in the health care industry.
Leslie Pelton is vice president at the Institute for Healthcare Improvement, which launched the concept of Age-Friendly Health Systems in 2018, along with the John A. Hartford Foundation.
She describes the effort as one in which every aspect of care, including mobility, mental health and medication, is centered on the needs and desires of the older adult.
Pelton says 3,700 sites across the US - including clinics, hospitals, and nursing homes - are now designated age-friendly.
She describes the system as "a counterbalance to ageism, because it requires that a clinician begins with asking and acting on what matters to the older adult, so right away the older adult is being seen and being heard."
That sounds great to Liz Schreier. Schreier is 87 and lives in Buffalo. She walks and does yoga regularly. She also has a heart condition and emphysema and spends plenty of time at the doctor. She lives alone and says she has to be her own advocate.
"What I find is a disinterest. I'm not very interesting to them," she says. "And I'm one of many - you know, one of those old people again."
She goes from specialist to specialist, hoping for help with little things that keep cropping up.
"I had a horrible experience with a gastroenterologist who said I was old, and he didn't think he wanted to do a scope on me, which was a little insulting," she says.
She later found one of his colleagues who would.
Schreier says navigating the health care system in your 80s is tough. What she and her peers are looking for from health care workers, she says, is kindness, and advice on how to stay active and functional no matter how old they are.