Section Branding
Header Content
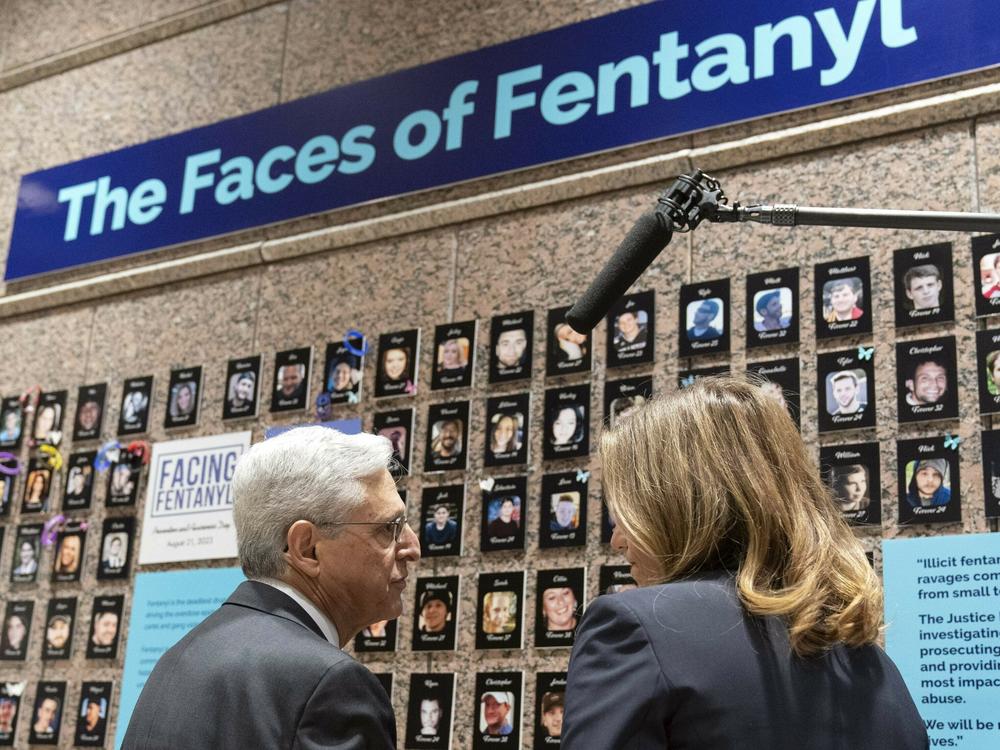
In 2023 fentanyl overdoses ravaged the U.S. and fueled a new culture war fight
Primary Content
When the history of the fentanyl crisis is written, 2023 may be remembered as the year Americans woke up to an unprecedented threat scouring communities - and a deepening cultural divide over what to do about it.
For the first time in U.S. history, fatal overdoses peaked above 112,000 deaths, with young people and people of color among the hardest hit.
Drug policy experts, and people living with addiction, say the magnitude of this calamity now eclipses every previous drug epidemic, from crack cocaine in the 1980s to the prescription opioid crisis of the 2000s.
"We've had an entire community swept away," said Louise Vincent, a harm reduction activist in North Carolina, who says she still sometimes uses street opioids including fentanyl.
"We do have fentanyl that's dangerous, we have xylazine that's poison," Vincent told NPR. "We've had an entire community swept away. I can't even think of all the people I know who have died. My daughter died. Our mentors are dead. It is so dangerous right now."
Public health experts say fentanyl, a synthetic opioid far more powerful than heroin, is responsible for the majority of drug deaths. But the supply of illegal drugs is increasingly complex and perilous.
Americans using drugs recreationally, or caught up in more serious addiction, face an unpredictable cocktail that often includes fentanyl, methamphetamines and fast-changing mix of new chemicals.
The latest threats include the horse tranquilizer xylazine, which causes lingering flesh wounds in users, and nitazenes, synthetic opioids that appear to be even more potent than fentanyl.
Often Mexican drug cartels press these chemicals into pills, which are counterfeited to resemble pharmaceutical-grade medications for ADHD, depression, and pain.
"This is why it's so important for you to understand that you cannot just simply pick up a drug and go ahead and use it," said professor Bonnie Halpern-Felsher, head of Stanford University's REACH Lab, which focuses on understanding, preventing and reducing teen and young adult substance use.
Federal researchers now say drug overdoses are a leading cause of death among young Americans age 18-45 and have also spiked as a killer of pregnant women.
The issue has become a major flashpoint for politicians, with many Republican politicians blasting the Biden administration for failing to stop fentanyl smugglers.
"We've had more Americans die of fentanyl than the Iraq, Afghanistan, and Vietnam wars, combined," said Nikki Haley, the former South Carolina governor who is now seeking the GOP presidential nomination, speaking to voters in New Hampshire on Dec. 14.
Hopes dashed for a quick solution to the overdose crisis
Drug deaths first began to soar in the U.S. in early 2020 - from an already devastating 65,000 a year - to what policy makers fear is a new baseline of more than 110,000 a year.
At first public health experts linked the carnage to the Covid pandemic, when lockdowns disrupted addiction treatment programs and heightened isolation.
But predictions that this new overdose crisis would fade as American life returned to normal have evaporated.
"It continues to go up," said Dr. Nora Volkow, head of the National Institute on Drug Abuse, the nation's top drug policy and addiction research agency, in an interview with NPR.
"I had been hoping after we emerged from the Covid pandemic, we would start to see it go down. It hasn't continued to rise as sharply, but it's rising."
In 2023 the overdose death rate topped 112,000 in a 12 month period for the first time, according to the Centers for Disease Control and Prevention.
Biden administration officials say they have "flattened" the upward curve.
But speaking this month during a press conference in Maryland, White House drug czar Dr. Rahul Gupta acknowledged the gravity of the public health crisis.
"We cannot treat dead people," he said.
According to Gupta, federal spending on the crisis has surged, with roughly 40% more dollars flowing to the states.
There have been other policy gains in 2023, including approval of over-the-counter-sales of naloxone, a medication that can reverse most opioid overdoses.
"We have to do more," Gupta acknowledged "We have to make that sure we're getting people the help they need [with addiction] and we have to go after the trafficking profits [of drug dealers]."
A U.S. drug death every 4 1/2 minutes and no quick fixes
Why aren't these policy responses doing more to help?
Experts point out that much of the government funding spent on to addiction in the U.S. actually goes to pay for law enforcement and drug interdiction, funding police, prisons and border security.
According to the Cato Institute, a libertarian think tank, total annual spending on the drug war now tops $40 billion a year.
Most drug policy experts agree this vast system failed to detect or stop the rapid spread of more toxic synthetic street drugs.
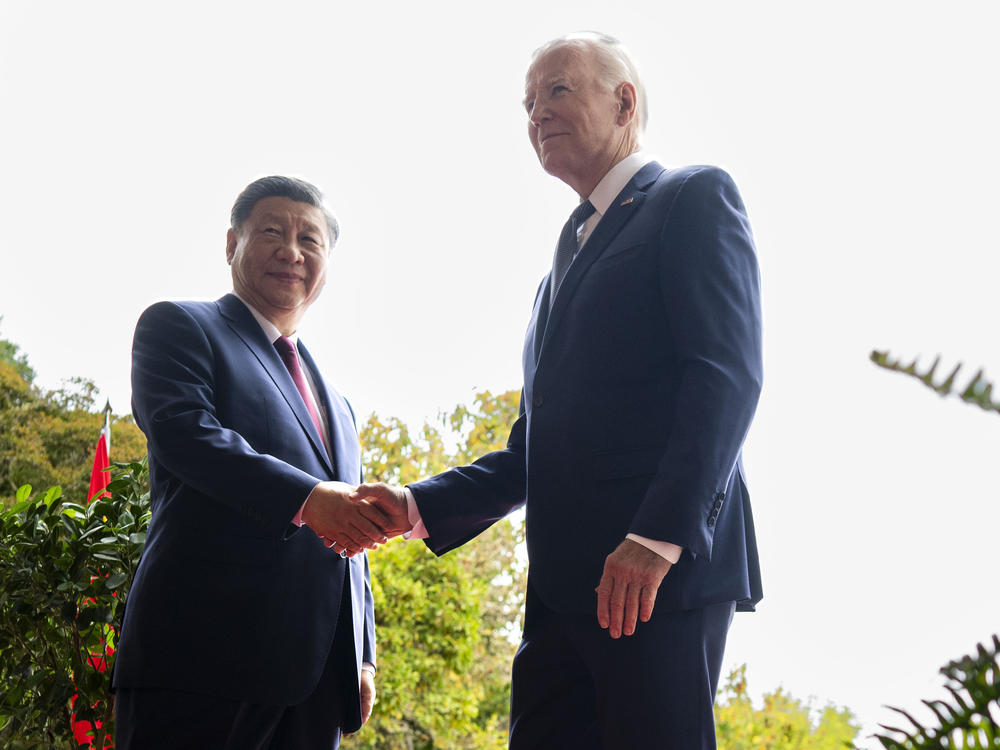
Efforts to weaken fentanyl production and smuggling by Chinese chemical manufacturers and Mexican drug cartels have failed to curb the supply in American communities.
According to the U.S. Drug Enforcement Administration, law enforcement seized "more than 360 million deadly doses" of fentanyl in 2023, but the drug remains cheap and widely available.
Meanwhile, the network of roughly 17,000 drug rehab and treatment centers across the U.S. is often described as a "wild west" of expensive, poorly regulated and unscientific programs.
Most offer abstinence-based care, which means people experiencing addiction can't get help until they're ready or able to stop taking drugs. Experts say that leaves millions of fentanyl-users - and people experiencing other substance use disorders - vulnerable.
In 2023, New Hampshire Public Radio highlighted the widespread dysfunction in the treatment industry, airing a podcast series The Thirteenth Step that investigated allegations of sexual abuse of clients in the drug treatment system.
"The [government] oversight that does exist, it's just not capable of finding unethical behavior like this," said NHPR senior reporter Lauren Chooljian in an interview with NPR.
As deaths soar, more families and communities turn to "harm reduction"
One more challenge is the mainstream medical community, which has largely resisted helping with the crisis.
Federal regulators have lowered barriers for doctors to use proven medical treatments for opioid addiction and overdose, especially buprenorphine and naloxone.
But a study published in July 2023 in the Journal of the American Medical Association found most physicians don't prescribe these medications to their patients.
Left with few options, many communities, grassroots organizations and families have turned increasingly to a strategy that's been used in other countries known as "harm reduction."
It's a healthcare approach designed to keep people alive while they use drugs, until they're able to enter into some kind of recovery.
Strategies include handing out naloxone; distributing clean needles and pipes so that people don't share equipment and spread disease; and offering basic medical care and counseling.
Some harm reduction workers also monitor people actively using drug use to help prevent fatal overdoses.
"People die of overdoses because they're by themselves," said Renae, a harm reduction worker who believes this approach can also reduce stigma and help healing.
"The stuff [access to safer drug use] is just the carrot I dangle before the horse, I'm wanting to make a connection," she told NPR.
NPR is not using Renae's full name because some of what she does to help keep people alive, like supervising active drug use, is illegal.
In 2023, a growing backlash against "de-stigmatizing" drug use
While programs like supervised drug use sites are widely accepted in Canada and parts of Europe, they remain controversial in the U.S. and the backlash against helping active drug users appears to be growing.
Voters decriminalized drug use in Oregon in November 2020, but the policy has since faced a sharp decline in popularity and many politicians and voters want to toughen the state's drug laws again.
In December 2023, one of the country's leading thinkers on drug addiction, Stanford University researcher Keith Humphreys, published an essay in The Atlantic arguing that progressive approaches to the fentanyl crisis have failed.
"Empathy for people in the clutch of addiction is noble, and finding ways to help them is a moral necessity," Humphreys wrote, along with co-author Jonathan Caulkins from Carnegie Mellon University.
They argue that destigmatizing drug use "is a profoundly mistaken approach" that fails to encourage users to seek full recovery.
Harm reduction advocates generally acknowledge their approach doesn't offer a silver bullet to the overdose crisis.
But many say they've been unfairly blamed for a drug epidemic that has spiraled out of control.
"We too are distressed by what we see in the street," said Kassandra Frederique, head of the Drug Policy Alliance, a group that advocates for decriminalization of drug use.
"While we do not agree with coercion or incarceration, we're also grasping to see what is going work. Not because it's some theoretical framework we're pushing but because we want it to work for our loved ones," she told NPR.
$50 billion in drug company money is slow to help the crisis
Another once-hopeful strategy for reducing drug deaths also appears to be tangled up in a growing muddle of political arguments and bureaucracy.
Over the last decade, drug companies that fueled the first wave of the opioid crisis by aggressively marketing and distributing pain pills, agreed to pay more than $50 billion in compensation to communities battling addiction.
But despite the urgency of the crisis, many states have left most of their funds unspent.
Some states, including Colorado and Rhode Island, have moved to invest more resources in programs like naloxone distribution and mental health programs for kids.
But many communities are spending the money on law enforcement budgets and on police equipment including patrol cars, roadside cameras and body scanners for jails.
That angers some family-members, including Carrie Spears in Ohio, who lost her 23-year-old nephew Tanner to a fentanyl overdose in 2021.
"It's not that I don't support law enforcement or first responders," Spears told NPR and KFF Health News. "But what research did they look at that said, yeah, surveillance equipment and canine [police units] help people get into recovery and sobriety?"
What comes next? The politics of fentanyl in 2024
Public health experts worry debates over how to help people in addiction survive and recover will intensify and grow even more divisive in an election year.
Democratic and Republican politicians have promised to stop or sharply curtail fentanyl smuggling from the Mexico into the U.S., but analysts tell NPR no one has proposed a plan that would accomplish that goal.
"The war on drugs hasn't worked," said Ioan Grillo, a Mexico City-based journalist considered an expert on the Mexican drug cartels, in an April 2023 interview with NPR.
"We've got more deaths from drug overdose than ever, we've got more violence between drug cartels in Mexico than ever."
Real solutions to the overdose crisis are likely to be complex, costly and time-consuming, especially if the street drug supply keeps evolving with more dangerous chemicals.
Experts say the most hopeful strategies will likely involve things like reforming healthcare, expanding access to housing and mental health programs.
Everyone interviewed for this story said doing that kind of work in 2024, at a time when Congress and the electorate are increasingly polarized, will be nearly impossible — even if drug deaths keep rising.
-Lee Gaines of WFYI, April Laissle of WFDD, and NPR Education editor Nicole Cohen contributed reporting for this story
Copyright 2023 NPR. To see more, visit https://www.npr.org.