Caption
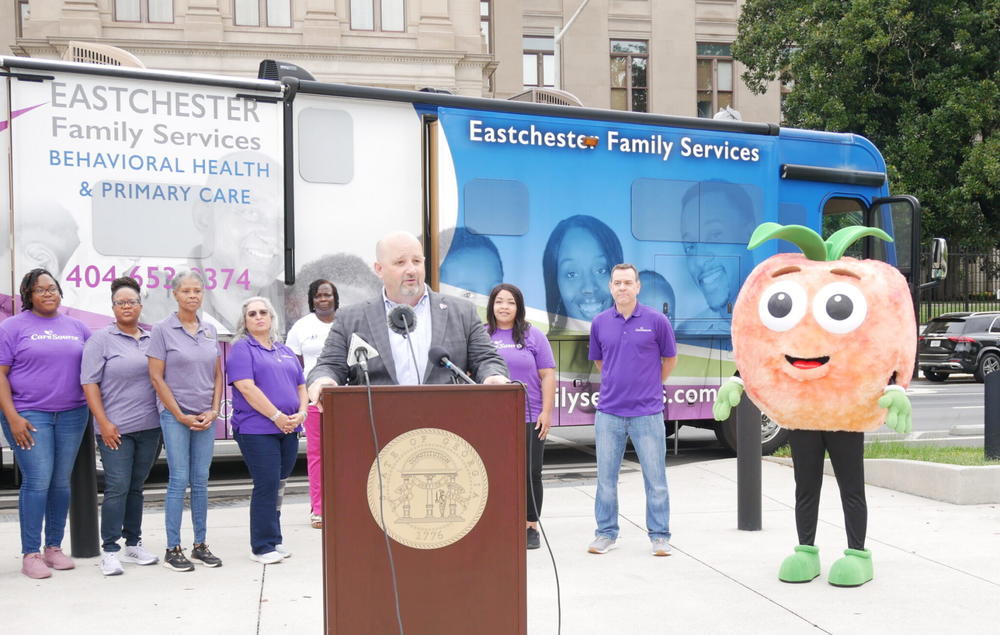
Jason Bearden, president of CareSource Georgia, talks about how the care management organization is using a mobile clinic to reach people at risk of losing their Medicaid coverage during the unwinding.
Credit: Jill Nolin/Georgia Recorder


