Caption
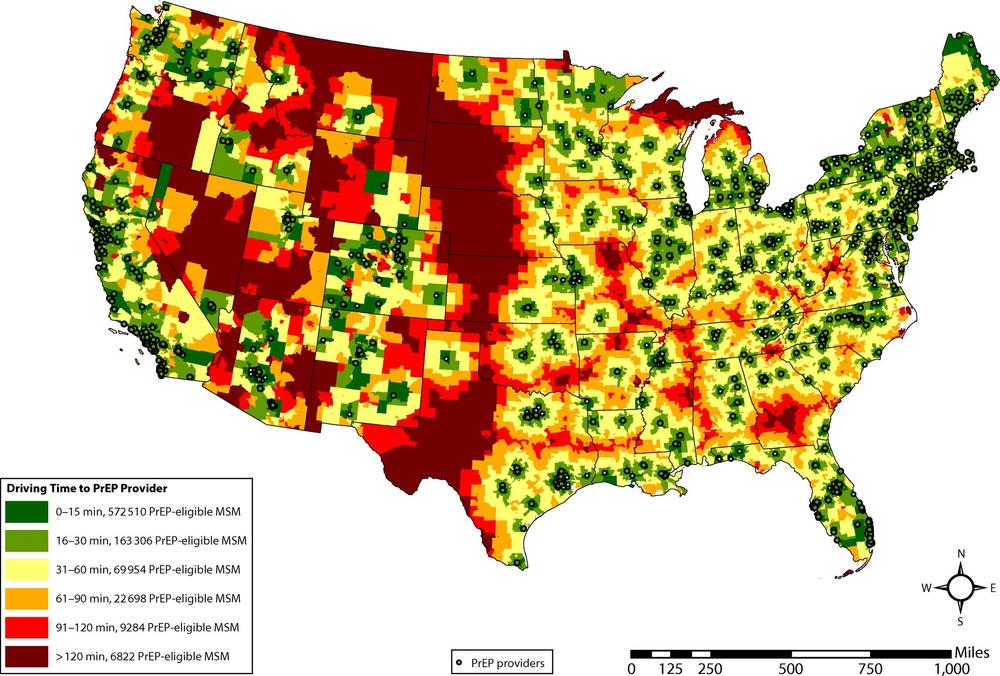
A map published in the American Journal of Public Health found that one in 8 PrEP-eligible men who have sex with men lived in 30-minute-drive deserts to pre-exposure prophylaxis, a highly effective medication in preventing HIV.
Credit: Aaron Siegler/American Journal of Public Health


